Sterilization forms and coding: documentation tips post ICD-10 implementation
Lori-Lynne A. Webb, CPC, CCS-P, CCP, CHDA, COBGC, CDIP
Originally published: March 25, 2016
Coding and reimbursement for sterilization has more to it than simply applying the CPT code, diagnosis code, submitting the claim and “voila” having the reimbursement dollars magically appear in the revenue stream.
The Federal Government has regulations in place that need to be followed for those providers that perform sterilizations and accept reimbursement from federally funded payers. These mandates are found within U.S. Code: Title 42 – The public health and welfare and are contained in the laws within Title 42. The sterilization consent form requirements can be officially found within; Title 42; Chapter I, Subchapter D, Part 50, Subpart B, Section 50.205. This is commonly referred to as “42 CFR 50.205 – Consent form requirements”
If you are a provider who performs sterilization procedures on a frequent basis, you are probably well versed in the process of getting this form filled out correctly and getting reimbursement. Many providers who only occasionally provide sterilization services are unaware of this mandated form, and either get the form filled out incorrectly, or don’t get the form filled out at all. This creates issues for the entire practice, and impacts the revenue you rightly deserve for providing this care. The requirement of this form is non-discriminatory, in the fact that it has to be filled out and utilized for those who perform sterilization procedures on men as well as those sterilization procedure performed on women.
50.205 Consent form requirements
“42 CFR 50.205” contains these parameters to be fulfilled
(a) Required consent form. The consent form appended to this subpart or another consent form approved by the Secretary must be used. link to federal form HHS-687
(b) Required signatures. The consent form must be signed and dated by:
(1) The individual to be sterilized; and
(2) The interpreter, if one is provided; and
(3) The person who obtains the consent; and
(4) The physician who will perform the sterilization procedure.
(c) Required certifications.
(1) The person obtaining the consent must certify by signing the consent form that:
(i) Before the individual to be sterilized signed the consent form, he or she advised the individual to be sterilized that no Federal benefits may be withdrawn because of the decision not to be sterilized,
(ii) He or she explained orally the requirements for informed consent as set forth on the consent form, and
(iii) To the best of his or her knowledge and belief, the individual to be sterilized appeared mentally competent and knowingly and voluntarily consented to be sterilized.
(2) The physician performing the sterilization must certify by signing the consent form, that:
(i) Shortly before the performance of the sterilization, he or she advised the individual to be sterilized that no Federal benefits may be withdrawn because of the decision not to be sterilized,
(ii) He or she explained orally the requirements for informed consent as set forth on the consent form, and
(iii) To the best of his or her knowledge and belief, the individual to be sterilized appeared mentally competent and knowingly and voluntarily consented to be sterilized. Except in the case of premature delivery or emergency abdominal surgery, the physician must further certify that at least 30 days have passed between the date of the individual’s signature on the consent form and the date upon which the sterilization was performed. If premature delivery occurs or emergency abdominal surgery is required within the 30-day period, the physician must certify that the sterilization was performed less than 30 days but not less than 72 hours after the date of the individual’s signature on the consent form because of premature delivery or emergency abdominal surgery, as applicable. In the case of premature delivery, the physician must also state the expected date of delivery. In the case of emergency abdominal surgery, the physician must describe the emergency.
(3) If an interpreter is provided, the interpreter must certify that he or she translated the
information and advice presented orally, read the consent form and explained its contents and to the best of the interpreter’s knowledge and belief, the individual to be sterilized understood what the interpreter told him or her.
information and advice presented orally, read the consent form and explained its contents and to the best of the interpreter’s knowledge and belief, the individual to be sterilized understood what the interpreter told him or her.
Critical verbiage and procedures
As you can see from the above, there are a lot of “rules” to be followed. However, the government has given us a standardized form to use and be implemented by the providers. They have even given us an electronic type version that can be downloaded and filled in, or even filled in on-line. This form can be found at http://www.hhs.gov/opa/pdfs/consent-for-sterilization-english-updated.pdf. This government form is currently valid for use though 12/31/2018.
The critical verbiage that must be followed closely is the mandate that “at least 30 days have passed between the date of the individual’s signature, and the date for when the sterilization is performed”. If this is not followed closely, the physician and the facility/hospital will not be paid.
This form is used across the United States, however, some State funded Medicaid programs may use their own form, but it has to contain the minimum information that has been outline in 42 CFR 50.205.
When implementing the procedure to get this form completed correctly, all staff, and especially the physician/provider, should be aware of its content and ensure that it is filled out correctly. This seems like more government buracracy however, if you are a Medicare/Medicaid provider this is part of the process we must perform to ensure the patient fully understands the implications of sterilization, and that as a patient they consent to the procedure.
ICD-10 diagnosing – ICD-10 procedure – CPT procedure
In the post ICD-10cm and ICD-10pcs world things have changed for the coding and reimbursement for sterilization codes.
In ICD-9cm we used code V25.2; Sterilization
In ICD-10cm we now use code Z30.2; Encounter for Sterilization
The codes are very similar, but in ICD-10cm they expanded the description to state that the usage of the code was for the encounter for sterilization – not just stating the word “sterilization” . So for the diagnosing of sterilization procedures it remains straightforward for the diagnosis of the sterilization procedure.
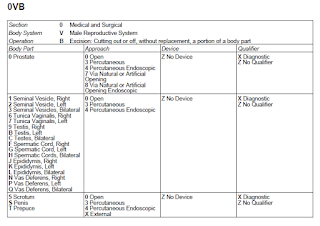
However, that is not the same for ICD10pcs. In ICD10pcs, the procedure of “vasectomy” is found in the index, and you’re referred to the code tables that provide the codeset for a procedure performed on the male reproductive organ system. The same can be said for the term “tubal ligation” as when you go to look it up the ICD-10pcs system as a tubal ligation, it refers you to the term “occlusion” where as you view the index, you find “Occlusion; Fallopian Tube; Left, Right, Bilateral” and refers you to the table sections that are appropriate. (see attached pages)
CPT procedures have many different codes that can be used for “sterilization procedures” so careful review of the operative reports to determine the correct code is a vital piece to ensuring your smooth reimbursement of sterilization procedures.
If you look in the CPT manual index, you will find the term for the “vasectomy”procedure, and CPT refers you to the numeric code of 55250. In the CPT codeset the code 55250 is found in the surgery/male genital system section under Vas Deferens; Excision; then the code 55250 is the only code that appears in this subset. If your provider does the traditional vasectomy procedure this is the correct code to use. However, there have been newer and less invasive techniques for “vasectomy” so code 55250 may not be the correct choice. It is this new technology that requires coders to carefully review the operative note(s) to ensure the correct CPT code goes with the correct diagnosis.
The same can be said for coding of sterilization for female patients. In the CPT manual sterilization codes for female patients can range from a very simple to extremely complex invasive procedures. CPT includes sterilization procedures that range from simple “incision” type procedure, and include codes for sterilization procedures that utilize laparoscopic technique, hysteroscopic technique, percutaneous incision, to abdominally open surgical procedures. CPT even includes codes that factor in a sterilization performed at the time of delivery (with a cesarean section) or even performed shortly after a vaginal delivery.
Diagnosis beyond “encounter for sterilization”
In cases where a sterilization is being performed, not all sterilization procedures are performed strictly for birth control. Providers, clinical personnel, and coders all need to ensure that the coding and documentation for a sterilization procedure is clearly reflective of why the procedure is being performed. Sterilization procedures may be required for a medically necessary or medically indicated diagnosis.
If a sterilization procedure is needed by the patient, this does not absolve us from not getting the proper paperwork filled out. (eg the federal sterilization form, appropriate consents, pre-authorizations, and referrals) In the case of a female patient requiring an emergent type of sterilization procedure, the 42 CFR 50.205 federal form allows for this circumstance in which the form still needs to be filled out, but the caveat of “emergency abdominal surgery” is noted on the form, and in the patients’ medical record.
When filling out the claim form for sterilization procedures that are not for contraceptive reasons, the medically necessary diagnosis would be appended first; then any additional medically indicated symptoms or diagnoses, with the final code of Z30.2; Encounter for Sterilization. When sequenced, this paints the picture of a medically indicated procedure, and denotes that the patient is also rendered sterile.
Prior to sending your claim, take the time to review the sterilization form and review it has been filled out correctly, all signatures and dates are correct and within the mandated guidelines. If the form is incomplete, or incorrect take the time to make all necessary corrections, and get all necessary signatures.
As you submit your claim, if it is an electronic claim, you may be required to submit a copy of the signed sterilization form, the operative report and also supporting medical records with your claim. If you are still submitting your claim as hard copy, you will need to include these documents as hard copy.
Final thoughts – wrap it up neatly
As a coder, you now have the unique opportunity to connect with your providers, clinical back office personnel, and your first line patient representatives to ensure that all the appropriate forms are filled out. You can provide the education and the importance of the sterilization form, and the importance of clear documentation to determine the reasons for the sterilization procedure. (eg, if done for “contraceptive or birth control” or “medically necessary/medically therapeutic” ).
If the sterilization procedure is denied for payment by the insurance carrier, review the denial code carefully, and if needed, contact the carrier to fully determine the cause of the denial. If warranted, appeal your denial.
For “male sterilization “ procedures performed in ICD-10 PCS
… for female sterilization “tubal ligation” procedures in ICD-10 pcs
Lori-Lynne A. Webb, CPC, CCS-P, CCP, CHDA, COBGC and ICD10 cm/pcs Ambassador/trainer is an E&M, and Procedure based Coding, Compliance, Data Charge entry and HIPAA Privacy specialist, with over 20 years of experience. Lori-Lynne’s coding specialty is OB/GYN office & Hospitalist Services, Maternal Fetal Medicine, OB/GYN Oncology, Urology, and general surgical coding. She can be reached via e-mail at webbservices.lori@gmail.com or you can also find current coding information on her blog site: http://lori-lynnescodingcoachblog.blogspot.com/.