Originally Published in MLN Connects
On August 2, CMS issued a final rule to update FY 2017 Medicare payment policies and rates under the Inpatient Prospective Payment System (IPPS) and the Long-Term Care Hospital (LTCH) Prospective Payment System (PPS). The final rule, which would apply to approximately 3,330 acute care hospitals and approximately 430 LTCHs, would affect discharges occurring on or after October 1, 2016.
The final increase in operating payment rates for general acute care hospitals paid under the IPPS that successfully participate in the Hospital Inpatient Quality Reporting (IQR) Program and are meaningful Electronic Health Record (EHR) users is approximately 0.95 percent. This reflects the projected hospital market basket update of 2.7 percent adjusted by -0.3 percentage point for multi-factor productivity and an additional adjustment of -0.75 percentage point in accordance with the Affordable Care Act. This also reflects a 1.5 percentage point reduction for documentation and coding required by the American Taxpayer Relief Act of 2012 and an increase of approximately 0.8 percentage points to remove the adjustment to offset the estimated costs of the Two Midnight policy and address its effects in FYs 2014, 2015, and 2016.
The final rule also includes:
• CMS-1632-F & IFC: Finalization of the extension of the Medicare-Dependent Hospital Program and low-volume hospital adjustment provided by MACRA
• Notification procedures for outpatients receiving observation services
• Hospital-Acquired Condition Reduction Program
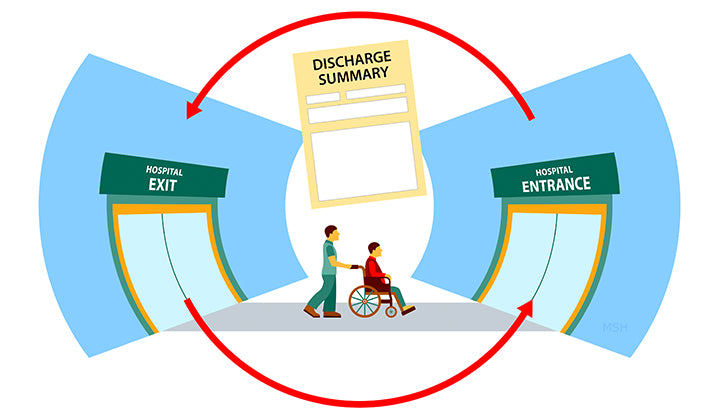
• Hospital Readmissions Reduction Program
• Medicare and Medicaid EHR Incentive Programs
• Hospital IQR Program
• Hospital Value-Based Purchasing Program
• PPS-Exempt Cancer Hospital Quality Reporting Program
• Inpatient Psychiatric Facility Quality Reporting Quality Reporting Program
• LTCH PPS changes
• LTCH Quality Reporting Program
See the full text of this excerpted CMS fact sheet (issued August 2).
The Medical Management Institute – MMI – Medical Coding News & MMI Updates




